Swine flu has made this a busy week for virus hunter Nathan Wolfe, who spoke at TED2009 about preventing the next pandemic. His groundbreaking Global Viral Forecasting Initiative (supported by grants from Google.org, the Skoll Foundation and others) monitors people in close contact with animals (such as subsistence hunters in central Africa) to catch new diseases before they spread. We caught up with Wolfe yesterday by phone, before his appearance on CNN with Anderson Cooper (who plays a cameo role in Wolfe’s TEDTalk), and asked him about this latest outbreak.
SARS, avian flu, swine flu … what’s going on here? Why are we suddenly seeing so many more outbreaks of viruses from animals?
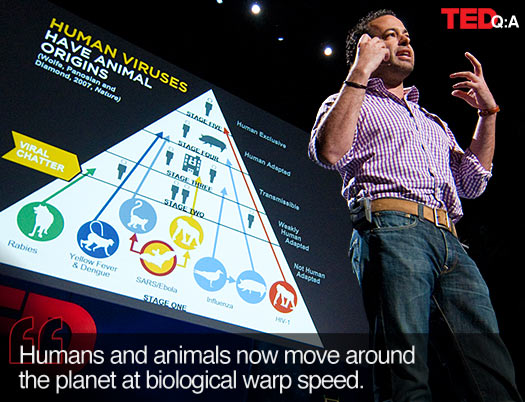
Viruses have always passed from humans to animals. In fact, the vast majority of human diseases have animal origins. But the human population is different from what it once was. For most of our history, we lived in geographically disparate populations. So viruses could enter from animals into humans, spread locally and go extinct. But the human population has gone through a connectivity explosion. All humans on the planet are now connected to each other spatially and temporally in a way that’s unprecedented in the history of vertebrate biology. Humans — as well as our domestic animals and wild animals we trade — move around the planet at biological warp speed. This provides new opportunities for viruses that would have gone extinct locally to have the population density fuel they need to establish themselves and spread globally.
We’ve created a “perfect storm” for viruses. And we’ll continue to see — as we have in the past few years — a whole range of new animal diseases as outbreaks in human populations. But we have to stop being surprised by them. Right now, global public health is like cardiology in the ’50s — just waiting for the heart attack, without understanding why they occur or the many ways to monitor for them, detect them early and ultimately prevent them. Swine flu is not an anomaly. We know that swine flu — like the vast majority of new outbreaks — comes from animals. We should be monitoring those animals and the humans that come into contact with them, so we can catch these viruses early, before they infect major cities and spread throughout the world.
Can we stop swine flu? Or is it too late?
If you catch one of these outbreaks early on, there may be the potential to do what we call containment, where you limit the outbreak to a particular site. But the reality is: By the time swine flu got on the radar screen of global public health, it had already spread. It was already in the States, it was in Mexico, it was in New Zealand. By the time it reaches that point, you’ve lost the ability to contain it. There are ways to decrease the spread of the pandemic, but by that point, it can’t be contained. (Editor’s note: See Larry Brilliant’s 2006 TEDTalk for more on the importance of early containment.)
The more fundamental question is: How do we prevent these pandemics from occurring? There are commonalities among all the pandemics that occur, and we can learn from them. One commonality is that they all come from animals. And the other commonality is that we wait too long.
At the Global Viral Forecasting Initiative, our approach is to take it a step back. If we can contain and monitor animal viruses at an earlier stage — when they’re first entering human populations, preferably before they’ve had a chance to become human-adapted, certainly before they’ve had a chance to spread — we can head off pandemics altogether.
Swine flu may or may not end up being an important human pandemic. But it’s a perfect illustration of the need for a paradigm shift in the way we approach global disease control.
In your TEDTalk, you lay out plans for monitoring humans who have close contact with animals in African jungles and Asian “wet markets.” Should you be monitoring pig farms as well?
Absolutely. What we do is all of the above. We monitor people with contact with wild animals as well as domestic animals. Chickens, ducks, pigs, monkeys … wherever people have contact with animals, that’s where we want to be, so we can catch potential pandemics at the moment that they’re born.
The good news is: For a variety of reasons, the percentage of the human population that’s in direct contact with animals is decreasing. So that gives us the potential to put a substantive percentage of that population into regular monitoring. Maybe we won’t catch everything, but we can create a much more substantive safety net for capturing these things before they go international or global.
READ MORE: Nathan Wolfe talks about why swine flu victims are dying in Mexico but not yet in the US; how swine flu is a “cosmopolitan virus”; and more … Your Global Viral Forecasting Initiative is expanding worldwide, but mainly in Asia and Africa. If you were in Mexico, how might things have gone differently?
In this case, we would have hoped to catch and contain swine flu when there were just dozens — instead of hundreds or thousands — of cases in Mexico, and before it spread globally.
GVFI’s objective is to monitor the portal of entry for new diseases into human populations — that means looking at the point at which humans and animals interface. We work with people who have high exposure to animals throughout the world, whether that means exposure to domestic animals — as with farm workers — or wild animals, as with people who hunt bushmeat in Africa or people who work in live animal markets in Asia. The minute we see new viruses that are entering into humans, we make this information available for the public health community, so we can develop drugs and diagnostics and potentially vaccines based on them.
When we see new diseases spreading in local communities, we monitor them very closely. If we were working in Mexico — and we were doing our jobs correctly — we would have caught this thing, perhaps in rural villages, before it made it to a site like Mexico City, and before it went international.
How do we understand the difference between the cases reported in Mexico, where many have died, and those in the US, which seem very mild?
There is a striking anomoly between what appears to be a very low rate of mortality and illness among the American cases and what appears, on the surface, to be a higher rate of illness among the Mexican cases. It could, of course, be the result of a difference in the viruses, although that doesn’t necessarily appear to be the case. It could be a difference in host populations, although again, that’s difficult to explain.
One possibility is that because we’ve looked more carefully for cases in the States, we’re more likely to see individuals who are mildly ill. We might find that if we looked more comprehensively in Mexico, we’d see the same number of people who were very ill — because they’re easy to find — and a much larger number of people who were mildly ill. That would reduce the actual rate of mortality to a much lower number, and that may be more compatible with what we would see if the number increased in the American epidemic.
As the number of cases climb worldwide, many people are comparing this swine flu outbreak to the 1918 flu pandemic. Is that an apt comparison?
Well, they both represent novel introductions of influenza into human populations that were capable of spreading substantively. The 1918 flu was notable in the sense that it spread comprehensively, globally, and it had a very high rate of mortality — affecting not only the very old or very young (who have weak immune systems) but also people in the prime of their lives, who are overcome by their body’s own immune response.
Whether or not this happens with swine flu remains to be seen. Initially, it does not appear to have the level of deadliness that the 1918 flu had.
I love bacon. Am I at risk?
Go ahead and have that BLT. It’s not a problem. You can’t get swine flu from eating pork. You’d have to have close contact with a living, breathing, infected pig to get this virus — or rather, in order to have contracted the original pig virus. The interesting and important thing about this “pig flu” is that it’s now spreading from human to human. It’s become a human virus.
So people should take the usual precautions: Stay away from individuals who are sick. Wash your hands frequently. And the less you touch your face, nose and eyes, the better.
Take us back a step or two: How did swine flu enter into the human population?
Swine flu has been known since at least the early part of the 20th century, since the 1930s. It was originally a virus of bird origin — all influenza viruses were originally bird viruses — and it probably spread to humans before it was in pigs.
Now, we still haven’t received definitive information on the underlying genetics of this particular virus. But initial reports suggest that it may be what’s known as a “mosaic virus,” which includes components of swine influenzas, bird influenzas and human influenzas. A cosmopolitan virus like that wouldn’t be unprecedented. (Editor’s Note: see Joe DeRisi’s 2006 TEDTalk for more on state-of-the-art virus detection.)
But in any case, this is a virus that appears to come from pigs, and pigs in close proximity spread the flu in much the same way that humans do — coughing, sneezing, and so on. The virus probably initially entered into human populations through people who work with livestock.
Is swine flu here to stay?
Whether this particular virus will sustain itself and become a permanent part of the human landscape is unclear, but that’s certainly what we’re watching for. As it is, the virus may just disappear because of the weather; summers aren’t good for flu viruses.
So this heat wave is working in our favor?
It might be. The virus has had a good start, from the flu perspective, considering that this is really the end of the season. But the unseasonably hot weather may bode poorly for this virus’ potential to establish itself definitively and cause a pandemic. Had this happened in September or October, it would be much more concerning.
Having said that, it’s not impossible that a virus like this might “go into hiding” — in the southern hemisphere or the tropics — and might come to light again next year. So there will be a lot of discussion about expanding the fall flu vaccine to try to control it next cycle.
Is it really possible for us to prevent future outbreaks like this?
Yes, I believe it is. We spend tons of money trying to predict complex phenomena like tsunamis, hurricanes, earthquakes. There’s no reason to believe that a pandemic is harder to predict than a tsunami. And we’d be foolish not to include forecasting and prevention as part of our overall portfolio to fight these pandemics.
Comments (11)
Pingback: Lekarska sujeta