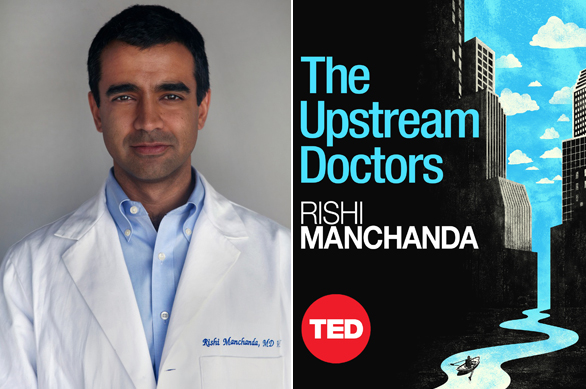
Rishi Manchanda answers questions about the new TED Book “The Upstream Doctors,” which looks at the environmental and social factors that play a big part in individual health.
We all think we understand the formula for keeping healthy — eat right, exercise, don’t smoke, skip dessert. But that picture is vastly incomplete, perhaps fatally so. In the eye-opening new TED book, The Upstream Doctors: Medical Innovators Track Sickness to Its Source, physician Rishi Manchanda says that while our individual health is highly dependent on our daily behaviors, it may be even more strongly influenced by the social and environmental conditions in which we live. Manchanda argues that the future of our health, and our healthcare system, depends on growing and supporting a new generation of healthcare practitioners who look upriver at the source of our health problems, rather than simply opting for quick-hit symptomatic relief.
These “Upstreamists,” as he calls them, are practitioners on the frontlines of health who see that health (like sickness) is more than a chemical equation that can be balanced with pills and procedures administered within clinic walls. They see, rather, that health begins in our everyday lives, in the places where we live, work, eat and play. Upstreamists — who may be doctors, nurses or other clinicians — know that asthma can start in the air around us, or from the mold in the walls of our homes. They understand that obesity, diabetes and heart disease partly originate in our busy modern schedules, in the unhealthy food choices available in our stores and even in the way our neighborhoods are designed. They believe that depression, anxiety and high blood pressure can arise from chronically stressful conditions at work and home. And, just as important, these caregivers understand how to translate this knowledge into meaningful action.
TED’s Jim Daly caught up with Rishi Manchanda to find out more about his philosophy. An edited transcript of their conversation follows.
You say medical care is just one of the components that shapes our health. What other forces determine how healthy we are as a society? In which areas are we deficient?
Experts often think of five general health-defining forces: genes and biology; behavior; medical services; social environment (the formal and informal ways we relate to one another); and physical environment. The latter two, often referred to together as the social determinants of health, are significantly more powerful drivers of wellness than medical care. The social determinants are shaped by the power and resources that people have, all of which are influenced by the policy choices we make as a society. These policies and our social and physical environment influence the behaviors and choices we make every day. The problem is that, with the current standard of care in medicine, healthcare often ignores and fails to alter these forces in order to help patients and communities lead healthier lives.
Is this a matter of life and death?
As a practicing physician, I think it is.
For whom?
In the book, I share the stories of patients with illnesses related to housing, transportation or hunger problems. Healthcare providers often treat symptoms for patients like these, but they don’t help connect patients to solutions that could address the root causes of their illnesses. So people often suffer unnecessarily for months, even years. And health care is not designed to intervene earlier and improve “upstream” social and environmental conditions and prevent illness in the first place. Recent evidence from the Institute of Medicine indicates that Americans — rich or poor, minority or not — don’t live as long as their counterparts in other rich countries, despite the fact that the United States spends more than any other nation on healthcare. In large part, this so-called “U.S. health disadvantage” is due to unhealthy social and environmental conditions in our neighborhoods. If we hope to get more value from our healthcare system, we must equip it to provide a better standard of care — one that can improve health where it begins.
That’s so interesting. Is it that the quality of the U.S. health care system is unevenly distributed?
Yes, there have been historically uneven levels of healthcare spending among regions and populations. But the ways in which individual providers and hospitals spend their healthcare dollars also plays a major role. While some choose to spend and practice wisely, too many providers and hospitals do not. They choose high-cost procedures, devices or drugs even when they’re not required and can expose patients to unnecessary risks or when lower-cost alternatives can provide the same results.
Another major and under-appreciated reason for variations in healthcare quality: In a nutshell, healthcare simply doesn’t do enough to understand or treat health where it begins — like where we live, work, eat and play. Providers and hospitals tend to do a poor job providing care that’s tailored to the social and environmental context of a patient’s life. This affects the quality of care, especially for populations that suffer higher levels of disease due to social risk factors, such as unhealthy housing or workplaces. Incentives shape all of these quality-related issues, from the national down to the neighborhood level.
In the book, you lay out a plan to transform our “high-cost, sick-care system into a high-value, health-care system.” What are the first steps you’d take?
We, as patients and providers, can take several important and immediate steps to radically improve healthcare. One step involves engaging clinicians to think about creating a better standard of care that considers the upstream forces that shape our health. The book lays out a framework and detailed steps to go about this work. In one of those steps, I describe a rating system that patients can use to assess and choose healthcare providers based on their demonstrated commitment to improve health where it begins.
The book notes that social and environmental forces on health are also capable of changing our DNA. How?
Epigenetics, an emerging field of science, examines the link between environmental exposures and the regulation of our genes, especially as they pass from one generation to the next. New discoveries in epigenetics now reveal that exposure to toxins, such as chemical pollution or even severe emotional stress, can significantly affect the health and development of individuals and their children. One study I discuss in the book showed that children born to mothers who experienced stress and psychological abuse during pregnancy were significantly more likely to have DNA changes that reflected a higher sensitivity to stress hormones, when compared to children of women who did not suffer abuse.
Many Upstreamists had some kind of early experience that opened their eyes to the social nature of health and medicine. What was yours?
Long before medical school, I had a chance to work in different settings, from rural India to immigrant, working class communities in the Boston suburbs. Both experiences allowed me to explore the intersection of health and social development. Along the way, I came across incredible role models and stories of communities that were able to dramatically improve health outcomes through civic participation, education and the promotion of policies and laws that focused on prevention.
When is it hard to be an Upstreamist, to go beyond diagnosing and prescribing and to tackle the root causes?
It’s hardest to be an Upstreamist when the business model in healthcare, which is typically based on a fee-for-service model, prevents clinicians and staff from getting the time, resources or support to tackle the root causes of disease. Still, there are great examples of present-day Upstreamists who have applied their leadership skills and creative talents to have some success in addressing root causes.
Which health care systems around the world do you admire? Which can we learn from?
Places like Kerala, a state in southwest India, have achieved significant health improvements by investing in an equitable distribution of primary care and prevention. We have much to learn from healthcare systems in these places about how Upstreamists work.
The Upstream Doctors: Medical Innovators Track Sickness to Its Source by Rishi Manchanda is available now. Get it on Kindle.
And check out Paul Farmer’s rousing endorsement for this important book »
Comments (6)
Pingback: Mid-point update from GE-NMF | NCI Womenternships
Pingback: Save the Date for Our 2014 Conference | California School Health Centers Association
Pingback: Tackling sickness at its source: An interview with TED Book author Rishi Manchanda | National Physicians Alliance